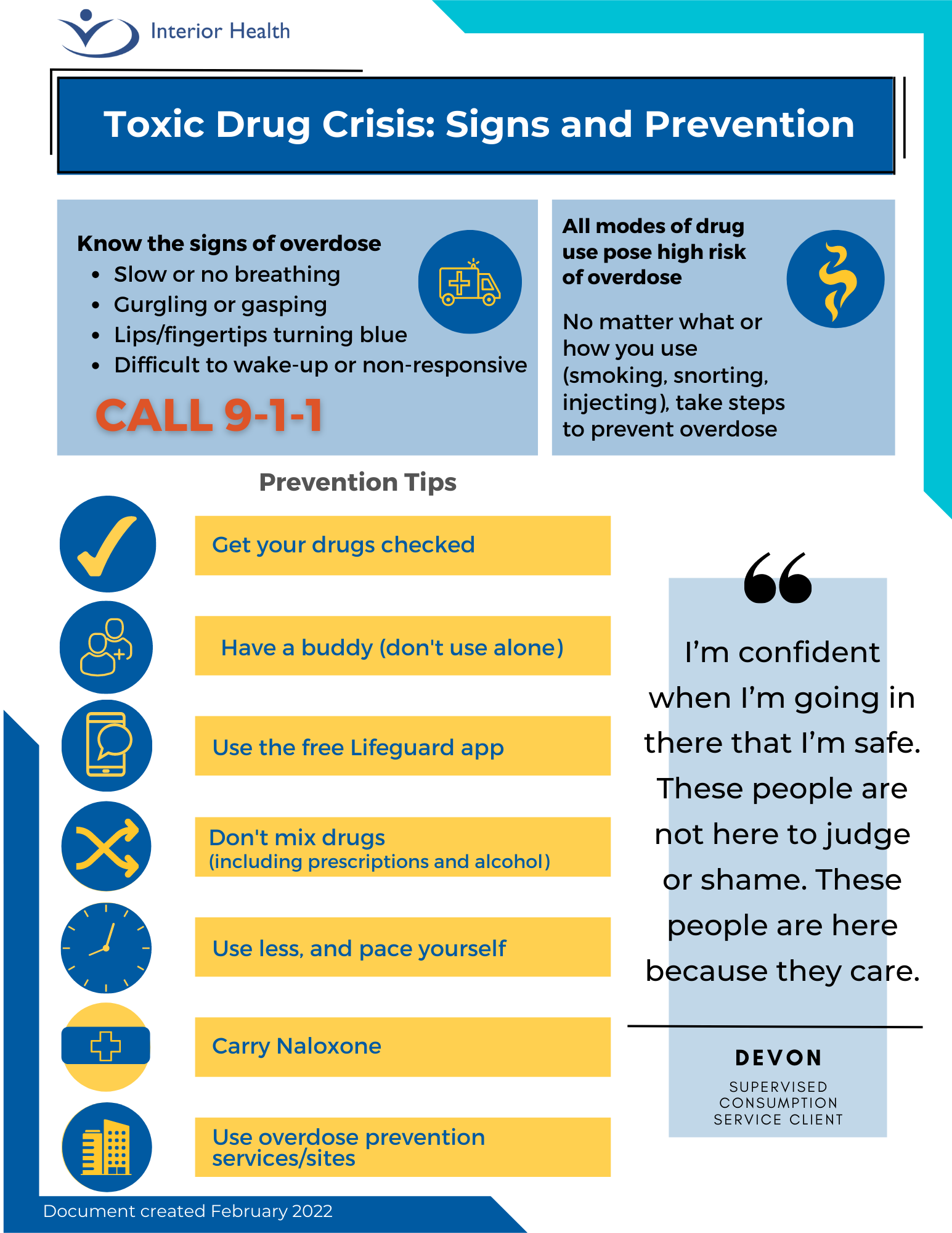
Need-to-know overdose information
- If someone is experiencing an overdose or is witnessing an overdose, call 9-1-1 immediately
- If you’re in crisis call 1-888-353-2273 for immediate assistance (24 hours, 7 days per week)
- View this infographic on toxic drug treatment options
- Get information about drug checking services in your area
- If you’re concerned about overdose activity in your community, visit our Harm Reduction page
- When there’s a drug or toxic drug alert, we will share the information on our Media Centre & Alerts page. You can also sign up to receive email notifications when there’s an alert or opt-in for text alerts through Toward the Heart by sending the keyword JOIN to ALERTS (253787).
- The drug supply is highly toxic and people who use drugs need to take precautions:
- Have a buddy or download the free Lifeguard app from the App Store or Google Play
- Don’t mix substances including pharmaceuticals and alcohol
- Use less and pace yourself
- Carry naloxone and know how to use it
- Access overdose prevention services and supervised consumption where available
- Recognize the signs of an overdose: slow or no breathing, gurgling or gasping, lips/fingertips turning blue, difficult to awaken, or non-responsive
- If someone is experiencing an overdose or is witnessing an overdose, call 9-1-1