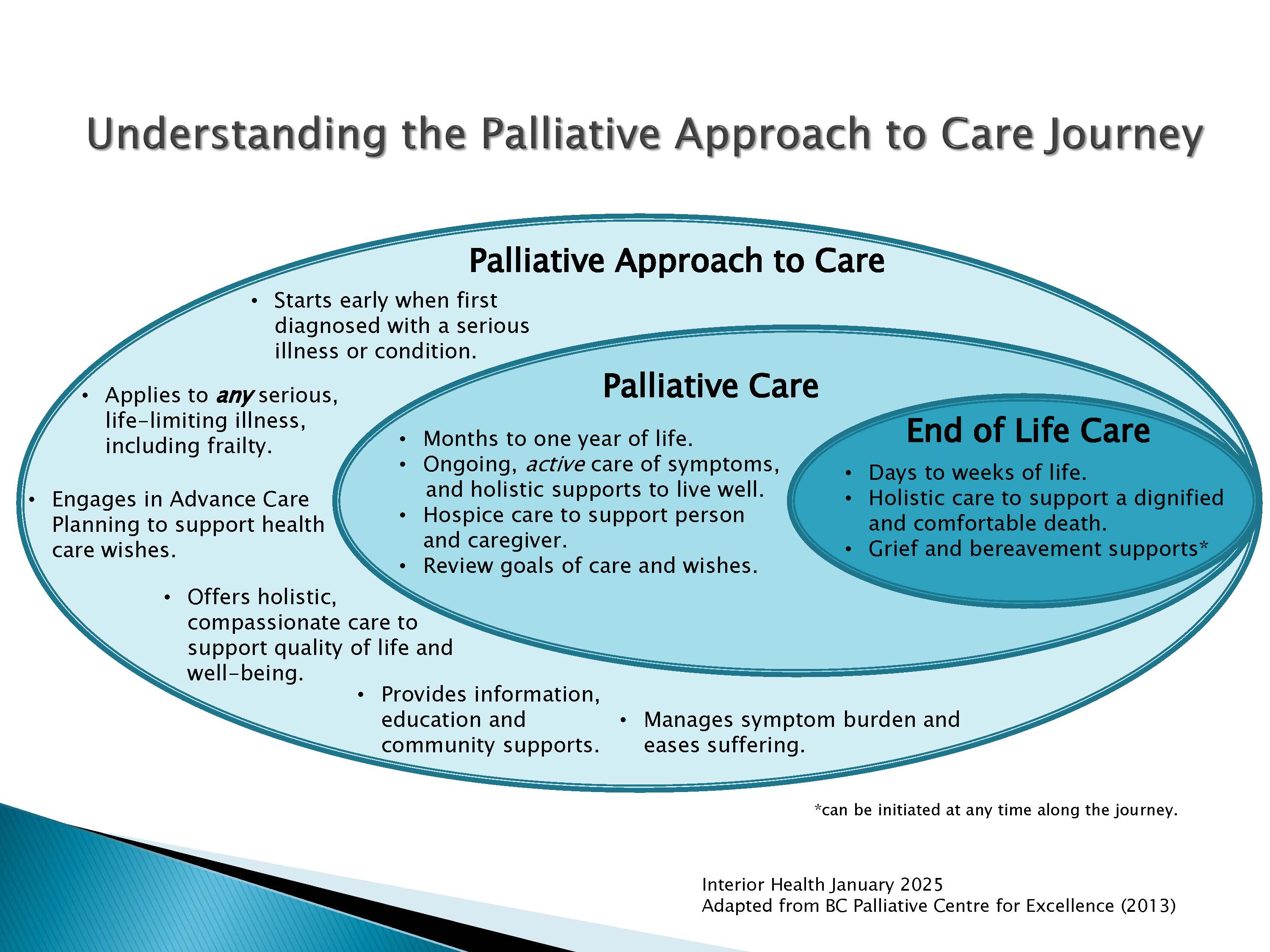
Palliative Care
Palliative care is an approach to care that supports the clinical, emotional and spiritual needs of individuals and their families coping with a life-limiting illness. Palliative care and a palliative approach to care focuses on comfort and support to the person and family, assists with making plans and decisions for the journey ahead, and optimizes quality of life. Sharing health care wishes and goals with loved ones, doctors and other health care providers is important.