Palliative care
These materials have been prepared solely for use at Interior Health (IH). IH accepts no responsibility for use of this material by any person or organization not associated with IH.
Access palliative and end of life care resources for health-care professionals.

These materials have been prepared solely for use at Interior Health (IH). IH accepts no responsibility for use of this material by any person or organization not associated with IH.
A wide variety of palliative tools and other resources are used within Interior Health that can help guide clinical problem-solving and decision-making for best practice palliative care.
The IH Palliative Care Nurse Consult Line is a service for Nurses who need an urgent consult with a Palliative Care Nurse for clinical assistance or direction for persons with palliative needs.
Copies of any palliative PPOs can be accessed through the PPO web page on the InsideNet, for those who have access, or by contacting the IH Palliative Care Office.
Clinical Decision Support Tools
Education - Public
Education - Staff
Education - Public
Learn more about evidence-informed guidelines that support best practice in Palliative and End of Life Care.
View resources that will support teaching individuals and families with palliative needs as well as recommended education for the expanded inter-professional palliative team.
Interior Health recognizes that Indigenous peoples in Canada experience health inequities as a result of the historical and ongoing impacts of colonialism. Culturally safe health care environments increase the quality of the health care services received, leading to increased service utilization and improved health outcomes. IH is committed to working with Indigenous partners and allies to create healthy and respectful care environments and practices which are safe and welcoming for all Indigenous peoples, their families and communities.
Many health-care providers are at different stages in their journey toward cultural safety and humility. There is information below and links to resources that support health-care providers in gaining knowledge, humility, and developing culturally safe practices.
A culturally safe environment is the desired outcome and can only be defined by the Indigenous person receiving care in a manner that is safe and does not profile or discriminate against the person but is experienced as respectful, safe and allows meaningful communication and service. It is a physically, socially, emotionally and spiritually safe environment, without challenge, ignorance or denial of an individual’s identity.
To be culturally safe requires positive anti-racism stances, tools and approaches and the continuous practice of cultural humility.
Cultural humility is a life-long process of self-reflection and self-critique. It is foundational to achieving a culturally safe environment. While western models of medicine typically begin with an examination of the patient, cultural humility begins with an in-depth examination of the provider’s assumptions, beliefs and privilege embedded in their own understanding and practice, as well as the goals of the patient-provider relationship. Undertaking cultural humility allows for Indigenous voices to be front and centre and promotes patient/provider relationships based on respect, open and effective dialogue and mutual decision-making. This practice ensures Indigenous peoples are partners in the choices that impact them, and ensures they are party and present in their course of care.’
Learn more by reading the report In Plain Sight: Addressing Indigenous-specific Racism and Discrimination in BC Health Care (2020)
Advance Care Planning (ACP) isn't just for older adults or people with serious illness, it's for everyone!
Initiating ACP conversations with patients can sometimes be challenging, yet are vital for ensuring that a person's preferences and wishes are known and honoured if they are unable to speak for themselves.
Interior Health has developed many ACP resources for both the public and health care providers. Please visit the following pages to access these resources, including the My Advance Care Plan workbook that can be ordered at no cost.
Visit our public Advance Care Planning webpage
Link to *internal Advance Care Planning page on the Medical Staff Hub
Link to *insideNet ACP page
*These internal links require login using IH credentials.

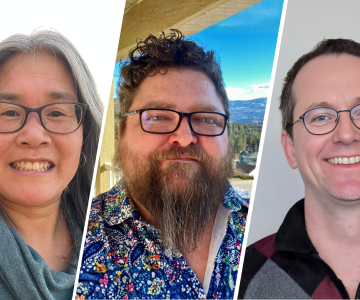
Shari, Maxwell, and Andrew work together across many different teams to provide sustainable, safe, and high quality facilities to patients and staff.
/stories/we-are-ih-staff-who-work-together-patient-comfort-safety


IH offers a range of services to help those who may have mental health, substance use or housing needs.
/stories/sharing-warmth-and-hope-ih-health-services-help-communities


Jayme helps ensure lived experiences are not just welcomed but embedded across Mental Health and Substance Use services at IH.
/stories/we-are-ih-coordinator-centres-peer-voices-care


As temperatures drop, it’s important to be aware of the health risks of cold. Here's what you can do to ensure you remain safe and healthy.
/stories/how-protect-yourself-and-others-when-temperature-drops


Heart disease is the number one killer of women worldwide and the leading cause of premature death in Canada. One in 3 women will be affected by heart disease.
/stories/how-women-experience-heart-disease-differently-men


Wavemakers is a free, groundbreaking virtual reality career-building program where post-secondary students can build skills and connect with employers like IH.
/stories/ih-helps-students-explore-careers-through-virtual-reality-program
Receive news, alerts, public service announcements and articles right to your inbox.
