Breadcrumb
Explore Stories
Health & Wellness
Interior Health (IH) delivers care through hospitals, clinics, long-term care homes, and other facilities. Behind the scenes many teams work together to keep these facilities safe, comfortable and sustainable.
They integrate key considerations such as HVAC systems, thermal energy priorities, and climate responsibilities into capital projects that support quality environments for patients and staff.
This includes managing how buildings use and generate energy to lower greenhouse gas emissions, and ensuring healthy indoor air quality.
Major infrastructure and energy projects rely on close collaboration across departments: Plant Services in partnership with Clinical Operations identify the needs and operational priorities, while the Project Management team plans, scopes and coordinates each project.
Once construction is complete, projects transition back to Plant Services, where regional plant managers oversee safe operations, maintenance and long-term performance.
Throughout the process, the Energy Management team provides expertise in efficiency, emissions reduction and sustainability. Together, these teams ensure IH facilities remain reliable, climate‑aligned and focused on protecting patient and staff well-being.
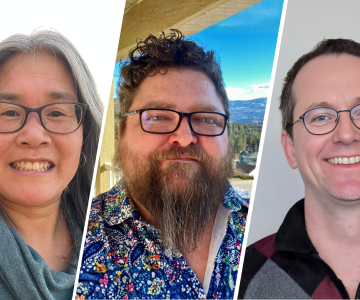
Meet some of the team members who bring this process to life and learn about their roles.
Community & Culture
In the interior of B.C., where winter can sometimes be unforgiving, the need for warmth goes far beyond temperature. It’s about dignity, safety and belonging.
For individuals who are unhoused or at risk, the cold season brings heightened vulnerability; not just to the elements, but to a range of health and emotional risks that are often invisible to the public eye.
The link between housing and health is undeniable. According to Public Health Ontario’s report on homelessness and health outcomes, people who rely on emergency shelters, winter response sites or outdoor spaces face higher risks of chronic illness, mental health challenges, substance-related harms and barriers to accessing care.
These risks aren’t about personal choices: they’re about circumstances, access and safety. Without stable housing, even basic health care becomes difficult to access.
Community & Culture
Name: Jayme Pereira (she/her/hers)Job Title: Coordinator, Peer InclusionLength of Service: 4Worksite: Kelowna Community Health and Services Centre (CHSC)Community: KelownaAncestral Territory: syilixFavourite Quote / Advice to Live By: “Everyone you meet is fighting a battle you know nothing about. Be kind. Always.” —Robin Williams
Jayme lives in Kelowna on the traditional, ancestral and unceded territory of the syilix Nation. For her, family and community guide how she navigates life. That sense of connection to people, shared experiences, and a responsibility to embody inclusion is something Jayme carries into work every day.
To Jayme, reconciliation is not a single action or statement. It’s a practice. It’s a way of life.
“Reconciliation starts with a commitment to learning the truths of the past, reflecting on my own assumptions, and building relationships rooted in respect and humility. I believe it is a lifelong practice, and I commit to showing up with consistency, curiosity and care.”
That commitment to listening, especially to voices that have too often been excluded, is central to Jayme’s work in the Peer Inclusion program—and the fuel for each choice she’s made along her career path.
Health & Wellness
After a warm and rainy start to winter across much of the province, British Columbians are encouraged to prepare for colder weather and winter road conditions in the days and weeks ahead.
As temperatures drop, it’s important to be aware of the health risks of cold. Here's what you can do to ensure you and your loved ones remain safe and healthy.
Health & Wellness
Heart disease is the number one killer of women worldwide and the leading cause of premature death in Canada. One in three women will be affected by heart disease.
Dr. Emmanuelle Massie is a cardiologist at Interior Health (IH) in Kelowna. “Cardiovascular (heart) disease is a leading cause of mortality in women,” she says. “However, most clinical trials have enrolled a much greater proportion of men compared to women, and hence there is very little data on women in this field.”
Community & Culture
Thanks to a free virtual reality tool, Interior Health (IH) is connecting with post-secondary students in new and creative ways to spark interest in health-care careers.
In partnership with Wavemakers, a national, Government of Canada supported initiative, IH connects with students from a wide range of educational backgrounds and creates opportunities for them to explore career pathways in a fully virtual environment.
IH, a Wavemakers partner since 2022, is one of the only health authorities in Canada participating in the program’s national career and networking events.
Apply to Wavemakers
Health & Wellness
Heartbreaking tragedies in our communities, province or even those far away from us can bring up a range of emotions: sadness, fear, anger and a sense of helplessness.
These reactions are normal. In times of collective pain, tending to our own well-being is not only important, but necessary.
We encourage anyone to reach out for support, whether for yourself, a colleague, or someone in your life who may be hurting.
Interior Health (IH) and our community partners provide mental health services for youth and adults. Our services are confidential and safe, and free of judgment and stigma.
Community & Culture
Interior Health is proud to collaborate with local Indigenous artist Johnny Mukwa, who has donated artwork to Kootenay Lake Hospital in Nelson.
In a deeply personal gesture, Johnny donated two art pieces, Forest Spirits 1 and Forest Spirits 2, to the hospital’s oncology department. They’re hung in the hallway where oncology patients and families will see them.
Community & Culture
We’re honoured to announce that Interior Health (IH) has been recognized as one of BC’s Top Employers (2026)—a distinction that celebrates organizations across the province that are shaping outstanding, people-centred workplaces.
This recognition reflects IH’s ongoing commitment to strong policies, meaningful career pathways, continuous learning, comprehensive benefits, a culture grounded in compassion, respect and support for our teams.
Creating a compassionate culture is a top priority at IH, one of B.C.’s five regional publicly funded health authorities.
-
Load More
Showing 9 of 837
Sign up for email updates
Receive news, alerts, public service announcements and articles right to your inbox.