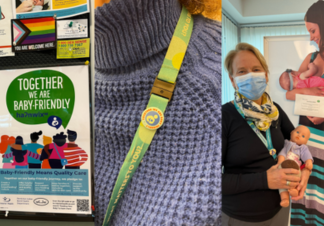
If you're having a baby in Penticton, you’re part of an international initiative to improve the care that families receive before, during and after the birth of their baby, thanks to the Baby-Friendly Initiative.
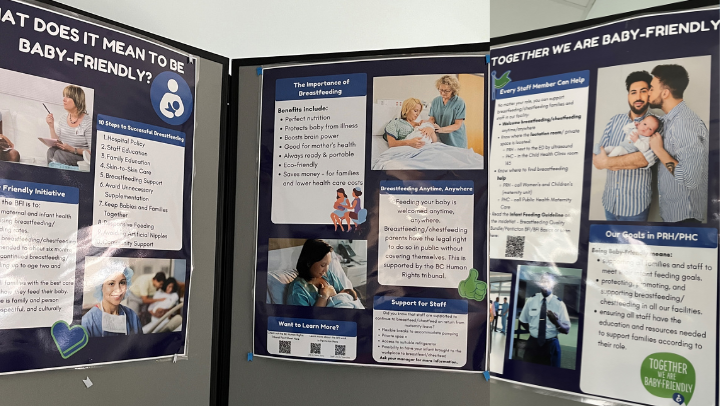
The Baby-Friendly Initiative, or BFI, is a World Health Organization and UNICEF program that guides health-care providers in breastfeeding best practices, and ensures families have the support they need and want.
In 2019, Penticton Regional Hospital (PRH) and Penticton Health Centre (PHC) collectively were one of only 25 sites in Canada to be chosen to pilot a BFI project. Now, three years later, PRH and PHC are on the cusp of receiving their baby-friendly designation thanks to the work of project co-leads Meggie Ross, Patricia Park and Cindy Barton.
For expectant families in and around Penticton, the designation means knowing they’re receiving optimal care that gives mothers, babies and families the best start in life.
As Meggie Ross explains, “The goal of BFI is to make breast and chest feeding easier for families by helping them get off to the best start possible, and supporting them for as long as they need. With BFI’s 10 steps to successful breastfeeding policies in place at our facilities, we know the family’s experience improves, and breastfeeding rates increase.”
If you or your family is having a baby in Penticton, this is what BFI means for you.