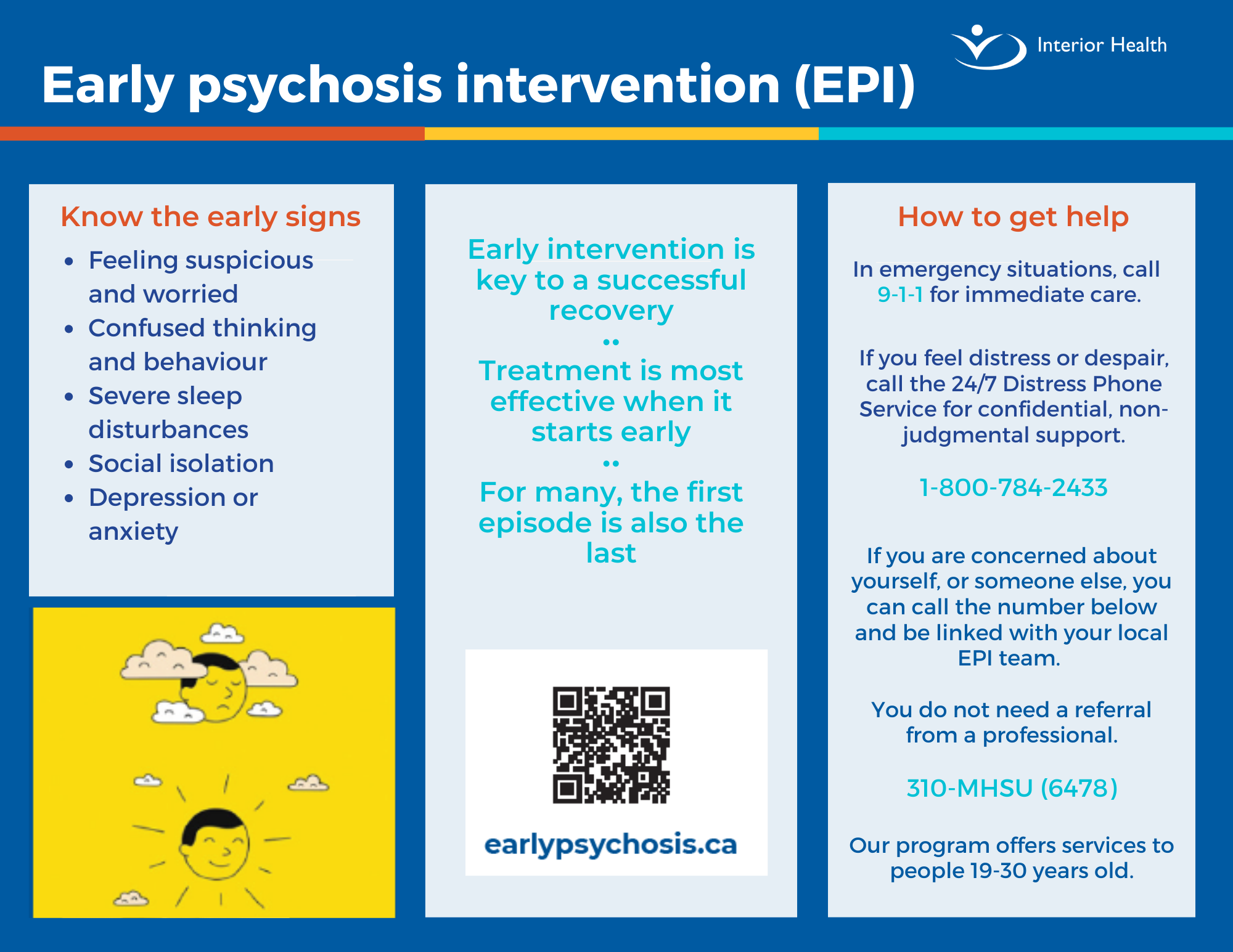
When you hear the word ‘psychosis,’ what words and images come to mind? Have you ever heard someone call something or someone else ‘psychotic?’
Psychosis can be a heavy-sounding word for what is a treatable mental health condition. Like many other mental illnesses, however, it also comes with stigma and shame.