Breadcrumb
Explore Stories
Health & Wellness
I’m already planning what I want to cook for the December holidays. I’m thinking of a dinner that’s a little less traditional this year and I'm looking at lemon risotto and stuffed squash recipes. I get excited about the holidays every year. For some reason cooking for celebrations is a completely different experience for me than the Monday to Friday grind of just getting a meal on the table.
As I was flipping through my cookbooks, my mind was drifting to all of the things that I take for granted and that I should give thanks for; things like being healthy and being able to afford the groceries for this meal.
Times are tough right now. More people are using food banks each year. I've been thinking about how difficult it must be to make a special meal when you're struggling to make ends meet.
People who don't have enough money to buy high-quality food are sometimes called "food insecure." Research shows that having enough nutritious food to eat is important to your health. Those who don't are more at risk of many health conditions including diabetes, heart disease, hypertension, back problems, and poor mental health. Kids with food insecurity have a higher risk of childhood mental health problems, asthma, and depression.
But why? Shouldn’t it be those folks planning rich holiday feasts who have a greater chance of heart disease? It turns out that it’s not that simple.
Not surprisingly, people who are able to buy healthy food are also more likely to have well-paid work, live in good neighbourhoods and afford a fitness pass. Living on a low income, having an unhealthy work environment, and paying a lot for housing, childcare and transportation are stresses that contribute to poor health. On top of all that, unhealthy, highly processed food is usually cheap, while fresh vegetables and fruit can be expensive.
It’s a problem with no easy fix. The good news is that there are many community organizations and local governments that are working to tackle these complicated problems, and Interior Health’s Healthy Communities Program is working alongside many of them.
Research & Innovation
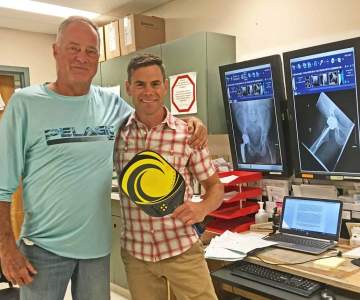
The little things were agony, says Gary Gierlichs.
“Little things, like putting your socks on or putting your leg in the car,” he says. “I deteriorated pretty fast, which was tough for an active person like me. Hip replacement changed my life—I can’t say enough about it.”
In 2018, Dr. Tim Bell and his surgical team performed a hip replacement on Gary at Penticton Regional Hospital using a relatively new procedure for Interior Health called the direct anterior approach. This approach allows the surgeon to replace the hip without cutting through muscle and tendon. As a result, patients like Gary experience less pain and are up and moving sooner, often on the same day as the surgery.
“I was thrilled when Dr. Bell told me I could play pickleball at seven and a half weeks after my surgery,” says Gary. “And I did—very gingerly, of course."
Dr. Bell is thrilled with the difference this procedure has made for his patients.
“What’s most enjoyable for me is seeing patients accomplish tasks after their surgery that they’ve been unable to do because of debilitating pain,” says Dr. Bell, who has now performed hundreds of these surgeries.
The direct anterior approach for hip replacement also adopts many of the elements of Enhanced Recovery After Surgery (ERAS). ERAS is an area of focus across Interior Health and uses evidence to minimize the stress of surgery and return the patient to their regular activity sooner.
For example, “drinking clear fluids close to the time of surgery gives the body energy to heal,” says Andrea Lindsay, a project manager for surgical initiatives at Penticton Regional Hospital. "Using narcotic and non-narcotic pain medications can also reduce or prevent nausea and delirium. And having the patient up and moving helps reduce the risk of muscle loss and the development of blood clots.
“If patients and their families are informed and prepared, they have less anxiety and a better experience.”
ERAS also includes lifestyle changes prior to surgery, for example, diet changes to reduce anemia, reducing smoking to reduce pneumonia risk, and strengthening the upper body in order to get in and out of a chair more easily.
“Hip replacement is still a major surgery, so it’s expected that patients will experience some level of pain. However, following some of the preparations of ERAS can reduce complications after surgery and shorten the time the patient needs to stay in hospital,” says Andrea.
And Gary? He’s now enjoying more activity than he has in years. Following his recovery period, Gary went on a holiday to Mexico, played pickleball three or four times a week, and rode his e-bike 60 to 70 kilometres a day.
Community & Culture
Stigma. It’s a word used to describe shame and fear of judgment.
It’s also the No. 1 barrier people with substance use disorders cite for not seeking help. And if you thought health-care providers are somehow immune and don’t carry prejudices, you would be wrong.
Like most health-care workers, RN Shari Smith* has dedicated her life to caring for people. Having spent years in critical care, she has seen the results of teen drinking, drug use and overdose. But she never thought it would happen to her family.
“I was so convinced in my mind that it could never be me,” the IH nurse says.
Her son had never had an easy time. He was dogged by health issues, struggled in school, and was labeled a “trouble-maker” from an early age. Still, he was an active kid who loved sports and had many friends.
“Then he had a car accident, and slowly drifted into drug use. Then he drifted in and out of the house. Then he was in and out of jail,” Shari says.
Finally, one warm summer evening after 10 months of abstaining from drugs, he overdosed while his family slept, thinking he was safe because he was with them at home.
“He’d been doing so well. I guess he wanted to celebrate and just do a bit. But it was a lethal dose of fentanyl.”
After the loss of her son, it took Shari a while to get back to work. She was acutely aware of the attitudes of those working at her side and words that stung like salt in a wound.
“We see overdoses every day, and you hear all kinds of comments. We had a young kid that had overdosed and the woman beside me was saying ‘what a waste of money – their parents should be given the bill because it’s their screw-up.’ Those comments are everywhere. Even from the nicest people. It’s so removed from them, they have no concept that it could happen to them too.”
When choosing to put a stop to stigma, words count. To learn more about using respectful language visit Toward the Heart.
*Names changed to protect privacy.
Community & Culture
At 66 years of age, Carolyn inspires those who know her. Born with cerebral palsy, Carolyn lived with her parents until their poor health made it necessary for them to move into a long-term care home three years ago. For the first time in her life, Carolyn needed to figure out the basics of living on her own. She learned how to cook, pay bills and make the 4.5 kilometre journey from her home to her parents' home on her power wheelchair. She makes this journey once a week to visit her parents, to get some help with her weekly bath, and help the activity team run their regular bingo game. Last winter, as the weather got colder, this routine started to become more difficult. Carolyn’s wheelchair couldn’t handle the long trip in the snow, and she didn’t have the money to use a transportation service anymore. “I’d been watching Carolyn for several months and was so impressed with her determination,” says Coreena Esser, a recreational therapy assistant at Interior Health's Adult Day Services program in Golden. “When I realized what a struggle she was having, I encouraged her to join the Adult Day program, so she could be picked up from her home and brought over for her bath, lunch and a visit with her family." Never one to leave well-enough alone, Coreena asked to visit Carolyn’s home later in the year to make sure she had the support she needed. “I noticed right away that the way Carolyn transferred herself from her wheelchair to the couch was very risky,” says Coreena. “I knew her knees wouldn’t be able to handle that motion for very long and I asked if she’d be willing to meet with our physiotherapist to see how we could make things better for her.” Through some trial and error with different walkers, and lots of hard work, Carolyn has a safe and effective way of transferring in and out of her wheelchair. Her work with the physiotherapy and rehab team had other benefits. Carolyn started using a stationary bike. As her strength improved, she was able to start walking for the first time in 15 years. “I’m so proud of Carolyn and all that she’s accomplished,” says Coreena. “She’s shown me that it’s never too late to learn something new.”
Community & Culture
For Helen Henderson, life is all about connections.
As kukpi7 (chief) of the Canim Lake Band near 100 Mile
House, she searches out connection to the land, to her band members and to her
past.
Earlier this year at Royal Inland Hospital (RIH) in Kamloops, several connections came together in one emotional ceremony for Helen, one of five Secwepemc kukpi7s who attended a sacred smudging ceremony at the construction site for the RIH Patient Care Tower.
It was her sister who was top-of-mind.
Helen and her sister Catherine were both born at RIH. Their mother travelled from the 100 Mile House area to give birth by caesarean section. After struggling for years with health and substance use issues, her sister passed away at RIH in 2011 due to complications from pneumonia.
“It’s bittersweet every time I go to Tk’emlups (Kamloops) because I have memories of my sister,” says Helen. “As hard as losing her was, it was almost like we were coming full circle in her journey. She was born on the fourth floor at RIH and she passed away on the sixth floor. I take comfort in the fact that that’s where her journey started and that’s where it ended. So as tough as it is to be in Tk’emlups, it also connects me with her.”
The smudging was performed in a private ceremony on a late afternoon day in October. A Secwepemc elder and knowledge-keeper performed the smudge while two drummers followed along, the sounds of a Secwepemc honour song echoing throughout the construction site.
Helen and her fellow chiefs bowed their heads in silent prayer. For her, the connection she feels is at the heart of the Secwepemc people.
“When I talk about connection and being connected to my
sister, I’m also talking about the connection to our ancestors,” she says.
“It’s only through that connection that we are able to carry on and build
strength in relationships. I know our mindset may be on a different level, but
at the root of our mindset is the health and well-being and healing of all
people. With the Secwepemc, that’s who we are: To be able to generate healing
for everyone, not just for our own people. That’s why it’s so special to be
able to bless a new build with a ceremony like this.”
Smudging is a traditional ceremony that involves the burning
of sacred herbs as part of a ritual, for cleansing or health purposes.
Secwepemc traditional wellness coordinator David Archie performed at the RIH smudging
as a drummer and singer.
“The smudge carries
our prayers, grief and loss and hands it over to the Creator and our ancestors
to take care of in a good way,” explains David. “This ceremony was held to
honour the ancestors of the Secwepemc people and was also a blessing for the
construction crews, medical staff and patients so they will be protected and
watched over while on site.”
As the drumming, singing and smudging came to an end, the chiefs, along with those in attendance, said a prayer and left behind a traditional offering of tobacco, known as a sacred medicine in Aboriginal culture.
Canim Lake kukpi7 (chief) Helen Henderson (middle) was joined by other Secwepemc Nation kukpi7s at a smudging event held at the Royal Inland Hospital Patient Care Tower in Kamloops. Also pictured (from left) are kukpi7 Patrick Harry (Stswecem’ Xgat’tem First Nation, Canoe Creek), kukpi7 Willie Sellars (T’exelc, Williams Lake Band), kukpi7 Rosanne Casimir (Tk’emlups te Secwepemc) and kukpi7 Sheri Sellars (Xatsull, Soda Creek First Nation).Helen says she was honoured to be invited to the smudging and be received by Tk’emlups Kukpi7 Roseanne Casimr on the ancestral lands of the Tk’emlups te Secwepemc. Kukpi7s were also in attendance from Xatsull, Soda Creek First Nation; T’exelc, Williams Lake Band; and the Stswecem’ Xgat’tem First Nation, Canoe Creek.
For Helen, being
able to connect the construction project to the Secwepemc culture was a special
moment.
“I know that being
able to practise our culture through the smudging can only bring health,” she
says. “It can only bring good things. When you start a new build, or a new
relationship, it’s based on ceremony and it’s based on our culture and because
of that it provides support to the building and to the structure. It also pays
respect to the ancestors we pay homage to on a daily basis.
“It is only through building our relationships
with Interior Health and with other organizations that we are even able to
start talking about reconciliation and what that would even look like. Doing
things like this is a really good step in the right direction.”
Health & Wellness
Does your teen vape? A recent Health Canada survey showed that 23 per cent of students in grades 7-12 have tried an electronic cigarette.
Health Canada has warned that vaping or using electronic cigarettes may cause health risks. Those health risks can be experienced by the person vaping, or by inhaling the vapours of others.
If you’d like to have a conversation with your teen about vaping, it's important to have the facts:
Vaping can increase your exposure to harmful chemicals.Vaping can lead to nicotine addiction.Although not all vaping products contain nicotine, the majority of them do, and some have the same or more nicotine than in a typical cigarette. Vaping nicotine can alter teen brain development.The ingredients typically found in vaping liquids include glycerol, flavours, propylene glycol and varying levels of nicotine… yuck! The long-term safety of inhaling these substances in vaping products is unknown and continues to be assessed.If you use tobacco or vaping products, be honest with your teen about the risks, and any regrets, difficulties and health effects resulting from your own experience. Talk with your teen about when and why you started to smoke/vape and explain how you thought it would make you feel, and how it is affecting your health.
Take advantage of situations
where you can talk to your teen about vaping. Odds are, you will probably need
to talk about the subject many times and in many different places.
Research & Innovation
Gina* is a tall, pretty young woman. Her hands, like much of her arms, are covered in ink. Her long hair is a shock of dreadlocks and her voice is not much louder than a whisper. But she is articulate and self-possessed and when she speaks, you lean in and listen.
Today she is speaking about her health troubles, her drug addiction, and how the injectable opioid agonist treatment clinic, or iOAT, has helped.
“The first month was really tough,” she says. There is a hint of pride in her voice. She has been attending the clinic regularly since it opened in April 2019.
“I’ve had people stop me and ask me what I’m doing differently, because I’m looking good. People at the shelter where I’m living think I work there. They think I’m a staff person,” she says.
She goes on to describe her volunteer work in the community. It’s clear that she enjoys helping others.
“Our injectable patients are really making dramatic recoveries, even though it’s early days,” says Dr. Megan Hill who runs the iOAT clinic. “We have had remarkable retention in the program since it started.”
The retention of clients is impressive because iOAT is a major commitment for people who typically have little stability in their lives. Clients need to attend three appointments each and every day to receive their medication. It is an obligation that they find worthwhile in order to receive medicine via injection in a safe, sanitary environment. The program can mean an end to the panic and chaos of street drug dependence.
“You get tired of the constant hustling and theft. The lies. That’s not who you are,” explains John*. “I don’t do that anymore. Best decision of my life.”
John has also been attending the iOAT clinic since it opened. He admits he is addicted to needles – not uncommon with severe opioid addiction – but he is also deeply concerned about the street drug supply, what is in the drugs, and how it’s impacting his health.
The iOAT clinic, he says, is a “10 out of 10” compared to other treatments he has tried.
“I’ve been to detox …” he pauses as if to count. “More times than I could even say,” he concludes.
Dr. Hill recalls one patient who told her ‘you guys care so much about my health that I decided I should too, and now I'm getting better.’ Another patient said, ‘I didn't think things could be good, but now they're starting to be good and I can address more problems than just my addiction.’
“Both have horrifying medical issues that have been completely unaddressed until now and it's hard to believe they've been living with them for so long,” says Dr. Hill.
The medication injected is called Hydromorphone. It is an opioid commonly used to treat moderate to severe acute pain. It helps with cravings for illicit opioids and prevents overdoses, as well as preventing debilitating opioid withdrawal, which is usually the reason people continue to use fentanyl or heroin.
The clinic also provides a regular connection with a health-care team, including physicians, nurses, pharmacists, and social program officers, which can help with overall stabilization.
For now John continues to take it a day at a time, spreading the word about the clinic and putting on weight.
“Because I’m living the good life,” he says, patting his stomach with a smile.
*Patient names changed to protect privacy
Health & Wellness, Research & Innovation
It's being called ground-breaking work.
A small and mighty team of Interior Health physicians and nurse practitioners are going above and beyond in supporting some of the region’s most vulnerable populations during the COVID-19 pandemic.
The devoted group are supporting people who are impacted by the poisoned drug supply crisis and have to isolate due to a positive COVID-19 test, by meeting them where they are.
An initiative led by the Mental Health and Substance Use Network brought together the group of health-care professionals who are providing coverage seven days a week to ensure people across the region have access to prescribed safer supply when needing to isolate.
“It is clear by the increasing death rates across the province that the drug supply has become even more toxic,” says Corinne Dolman, Interior Health's Manager of Substance Use Services. “This service is imperative not only to ensure people are able to isolate and reduce the transmission of COVID-19 but also to prevent high risk withdrawal from substances.”
The program has already worked with people in Vernon, Penticton, Trail, Kamloops and other parts of the region who may be at increased risk of overdose, withdrawal, cravings and other harms related to substance use.
“This vulnerable population has suffered increased isolation and stigma throughout the pandemic. The hard work and efforts to provide prescribed safer supply and other treatment medications has truly made all the difference. We have been able to reach this at-risk group and create connections for ongoing support that many did not have before,” says Pam Ruby, Interior Health’s Regional Pandemic Health Coordinator.
The program will continue until December 31, 2021.
“This is an innovative strategy that allows the vulnerable population to isolate with the added benefit of connecting the clients to addictions and harm reduction services across the entire region. This reduces barriers to care allowing the vulnerable population access to this much needed service. This is a ground-breaking innovation,” said Brent Hobbs, MHSU Network Director for Pandemic Isolation Centres.
-
Showing 791 of 791
Sign up for email updates
Receive news, alerts, public service announcements and articles right to your inbox.