Breadcrumb
Cold Weather
Be safe when the weather gets cold. Be aware of cold advisories in our region, and how cold impacts health.

Key information about cold weather and health
To access weather information and alerts for the Interior region, please visit Canada.ca/Weather or download the WeatherCAN app or Alertable,
Environment and Climate Change Canada has launched colour-coded weather alerts to help Canadians stay safe during severe weather. With this new system, all weather alerts—Warnings, Advisories, and Watches—are now colour-coded to reflect the level of risk. Learn more about colour-coded weather alerts at Canada.ca/Weather-Alerts.
- Prepared BC Severe winter weather and storm preparedness guide
- BCCDC Preparing for Cold Weather Events
- BCCDC Supporting People Experiencing Homelessness
- BCCDC Public Health Recommendations to Reduce the Impacts of Exposure to Winter Weather on People Experiencing Homelessness in British Columbia
- Cold Weather Exposure | HealthLinkBC
- Your health this winter | HealthLinkBC
- Staying Warm and Safe this Winter | First Nation Health Authority
- Extreme Cold | Health Canada
Cold and winter weather overview
Winter weather can affect one’s safety in many ways. Snow, rain and ice can cause transportation challenges and increase the risk of slips and falls. Power outages can disrupt communication, ability to heat your home and access to food and water.
Cold weather poses significant health challenges. These challenges impact many community members, and disproportionately impact people who are unhoused and underhoused, even in relatively mild weather conditions.
If a person is not able to be sufficiently protected from exposure to the cold air, wet weather, and wind for prolonged periods, cold related injuries such as windburn, trench foot, chilblains, frostbite or hypothermia may occur. Data from emergency departments across Interior Health showed that most cases of hypothermia occurred at temperatures of 0 degrees Celsius (°C) or colder. Trench foot and chilblains can even occur from exposure to mild cold conditions (generally 0 to 15°C) when combined with wet conditions.
Those at higher risk
Anyone can experience cold-related injuries when exposed to cold weather, but certain groups are at higher risk for frostbite, hypothermia, and other health impacts, including:
- People who are unhoused or underhoused
- People who are unhoused or underhoused are at the highest risk of death and injury due to prolonged exposure to cold weather as they often face multiple risk factors, further compounded by untreated underlying health conditions and inadequate access to winter clothing and sheltering.
- People living in inadequate housing without adequate insulation, or without adequate electricity or heat
- People who spend long periods of time outdoors for work or recreation, or transportation
- People who use substances, such as alcohol and opioids, that modify their ability to feel the effects of cold exposure
- People who are not dressed properly, having wet skin or wearing wet clothing
- People with disabilities or limited mobility
- People who live alone or are socially isolated
- People taking medicines that affect regulation of body temperature.
- People with certain medical conditions such as diabetes and peripheral neuropathy (muscle weakness, tingling, numbness), and diseases affecting the blood vessels
- People with mental health conditions
- Older adults (over 65 years of age)
- Infants (under 1 year old) and young children
Cold weather and health
Above freezing cold related injuries (0 C-15 C)
Chilblains is a skin condition that typically appears 12 to 24 hours after prolonged exposure to cold or damp conditions. It commonly impacts fingers and toes. To prevent chilblains, wear mittens, thick socks and weather appropriate footwear.
Symptoms
- Red or purple patches on the fingers or toes.
- Skin may feel itchy, tender, or firm to the touch.
- Blisters can develop in some cases and may become infected if not treated.
What to do
- Keep the affected area warm (e.g., wear gloves or insulated socks) and avoid further cold exposure so the skin can heal. It usually resolves on its own within a few weeks if the area is protected from further exposure.
- Seek medical attention if you notice blisters, increasing redness, or worsening pain, as these may be signs of infection.
Trench foot occurs after prolonged exposure of the feet (and sometimes the hands) to cold, damp conditions, typically between 0 C and 15 C for two to three days or longer. To prevent trench foot, wear waterproof, well-fitting footwear and change socks frequently to keep feet dry.
Symptoms
- Early signs: feet or hands appear pale or white, numb, and feel soft to the touch
- After rewarming: the area may become red, swollen, and very painful
- Blisters may develop in some cases
What to do
- Move indoors to allow the affected area to warm gradually at room temperature and let it air dry. Majority will recover with rewarming and proper wound care.
- Seek medical attention if the area becomes red, painful, or develops blisters, as these can lead to infection if untreated.
Below freezing cold related injuries (below 0 C)
Frostnip and frostbite occur when your body is exposed to the freezing cold within minutes to hours depending on circumstances and personal risk factors (for ex, pre-existing vascular disease). Exposed body part will have ice crystals forming inside, causing deaths of the tissue surrounding it. Frostnip is milder and can resolve after rewarming without permanent tissue damage. In frostbite, the exposed body part had been frozen and will leave permanent damage even after rewarming. To prevent, dress in layers (not too tight), and cover all exposed skin with mittens, thick socks, scarf or face cover and wear googles to protect the eyes.
Affected body parts
- Hands
- Feet
- Nose
- Ears
- Cheeks
- Chin
- Cornea
All frostbite should be evaluated by a health care provider. Start warming the area of skin impacted by frostbite when you know the person will be able to stay warm for a significant period to avoid greater tissue damage from re-exposure to cold after thawing.
What mild frostbite looks like
Skin can look yellowish or white but feels firm and waxy to the touch.
What to do for mild frostbite
- Passive warming - move to a warm room, remove wet clothing, wrap yourself in blankets or reheat your body by skin-to-skin contact by placing the affected body part under the armpit, for example.
- Active warming - This should be done at a health care facility under care of a physician where they may warm the frostbitten area. Thawing frostbitten skin could be painful. Do not rub, massage or shake the injured skin because that can cause more damage.
What severe frostbite looks like
Skin may be more discolored or may turn black. You may experience loss of sensation and see blistering.
What to do for severe frostbite
- Severe frostbite requires immediate medical attention. While you are waiting for help to arrive begin treating it with passive warming.
People are at risk of hypothermia when their core body temperature drops significantly below 35 C.
If you think someone may be hypothermic
- If they are cold, shivering, alert and complaining call 8-1-1 for advice.
- Take the person's temperature, if possible. If it is below 35 C, the situation is an emergency, get medical attention immediately or call 9-1-1.
- A person with severe hypothermia may be unconscious and may not seem to have a pulse or to be breathing. In this case, handle the person gently, call 9-1-1 and get emergency assistance immediately.
- Call 9-1-1 if in doubt about whether a person has hypothermia
There are three stages to hypothermia:
Stage one
Shivering, goose bumps on your skin, and numbness of extremities. Your breath can become quick and shallow, and you may feel tired and/or sick to your stomach.
Recommended actions
- Find shelter
- Keep your muscles moving
- Keep your body dry and (gradually) warm your body
- Remove wet clothing
- Wrap yourself in blankets/dry clothing
- Reheat your body through skin-to-skin contact with another person
- Drink warm, sweet beverage (non-alcoholic)
- Don't fight shivering, this is one of the ways your body increases its core temperature
Stage two
Shivering is more aggressive. Muscles are uncoordinated and movements are slow and laboured. You may suffer mild confusion, become pale, and your lips, ears, fingers, and toes may turn blue.
Please seek immediate medical attention and/or call 911 .
Stage three
If body temperatures drop below 32 C, the shivering will stop but a person may have trouble speaking, thinking, and walking. They may even develop confusion or loss of memory. When body temperature drops below 30 C exposed skin becomes blue and puffy, it will be hard to move muscles and behavior becomes irrational and more confused. A person's heart may be beating quickly but the pulse and breathing will decrease. In the most severe cases, there may be symptoms of unconsciousness, lack of pulse, or lack of breathing. At this stage there is a risk of dying.
Please seek immediate medical emergency and/or call 911
While waiting for medical care, begin warming yourself or the person you are with, as follows:
- Move to a warm room or shelter
- Remove any wet clothing
- Warm the center of the body first including chest, neck, head, and groin. To warm yourself, use an electric blanket (if available), warm water bottles, heating packs, and reflective blankets. Or in situations where external sources of heat are unavailable use body heat under loose, dry layers of blankets, clothing, towels, or sheets.
- Warm non-alcoholic beverages can help increase body temperature. Do not try to give beverages to an unconscious person.
After your body temperature has increased, stay dry and wrapped in a warm blanket, including the head and neck.
Windburn occurs when cold wind removes the top layer of oil from the skin causing:
- excessive dryness
- redness
- soreness
- itchiness
Recommended actions:
- Do not scratch or rub the affected area as it can damage the skin.
- Apply a protective skin care product (e.g. therapeutic moisturizers) to the affected area(s) as needed to help relieve the symptoms of windburn.
- Use a protective lip balm to treat lips.
Other health impacts
Cold weather can aggravate certain respiratory illnesses such as asthma, chronic bronchitis, and emphysema. The health of those with cardiovascular illnesses can also worsen due to cold. People with angina or those who have already suffered a heart attack or stroke can experience worsening of symptoms such as:
- Chest pain or pressure
- Increased heart rate
- Shortness of breath
- Increased blood pressure
The shorter, darker days of winter can get us down. Winters can be colder than usual, and people can feel more isolated if it is not safe to go out.
Staying indoors most of the time can make us feel tired and lower our mood and self-esteem. Here are some tips to stay positive in the winter season. Here are some tips to take care of your mental health during the winter season.
Learn about diagnosis and treatment of Seasonal Affective Disorder from HealthLinkBC.
Support and resources:
Preparing and responding to cold weather
- Bringing an emergency kit if you are going into the backcountry so you are prepared for conditions.
- Head for shelter that will protect from wind and rain.
- Avoid too much activity and sweating.
- Avoid touching metal.
- Eat and drink water.
- Avoid alcohol, caffeine, and nicotine.
- Wear proper clothing and keep dry.
- Cover your head and body by wearing a hat and layers of tightly woven fabrics such as wool or synthetics.
- Cover up exposed areas such as your fingers, cheeks, ears, and nose.
- Mittens are better than gloves at keeping hands warm and dry.
- Dress in layers so that you can adjust to changes as you heat up or cool off.
- Don’t wear tight fitting clothing or footwear that may impair circulation.
- Wear glasses or goggles if you are planning outdoor activities.
- If your clothes get wet, change into dry clothes as soon as possible.
- Bring additional warm clothing when going out for extended periods or in case of emergency.
- Talk to your health care professional to see if you are at an increased risk from extreme cold due to a medical condition.
- If you have health problems such as a heart condition you may wish to avoid strenuous activities like shovelling snow.
- Please ensure to have carbon monoxide detector in your indoor space.Look for ones with a Canadian certification mark (e.g., CSA, cUL, ULC or cETL).
Being prepared for winter weather is important. Thinking ahead and creating an emergency plan with winter-specific considerations will strengthen your ability to respond and recover.
Learn more about how to prepare for winter weather with these tools:
Severe weather can cause power outages. Be prepared for up to one week by developing a household emergency plan and putting together an emergency kit. If you encounter a downed or damaged power line, assume it is live and a danger. Stay back at least 10 metres (the length of a bus) and call 911 immediately to report it.
It is important to note that people can be at risk from cold and winter weather even when Environment and Climate Change Canada has not issued an alert. This is especially true for people at higher risk of cold-related injuries.
Learn more about preparing and responding to cold weather in BCCDC: Preparing for cold weather events.
Warming centres may be opened for the public by First Nations and local governments in response to cold weather events.
Temporary winter shelters and extreme weather response shelter spaces are funded by BC Housing and operated by community partners for people who are unhoused or underhoused. To find a shelter or warming space in your area, visit BC Housing’s emergency shelter listings.
During cold weather events, emergency warming centres and general warming space locations may be listed on EmergencyMapBC.ca at the discretion of First Nations and local governments. If warming centres are not listed on the map in your area, contact your Band office or local government.


For nearly three decades, Joanna Norman has walked alongside families during some of the most profound moments of their lives.
/stories/celebrating-passionate-midwife-international-womens-day


Small changes in your kitchen can lead to big benefits for your heart. Our video series shows how you can eat and live well using plant-based protein recipes.
/stories/how-cook-your-way-healthy-heart-plant-based-proteins

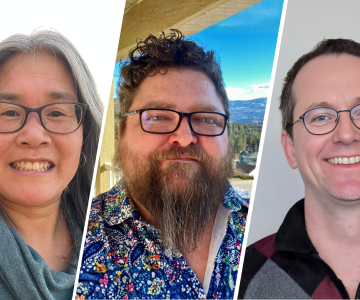
Shari, Maxwell, and Andrew work together across many different teams to provide sustainable, safe, and high quality facilities to patients and staff.
/stories/we-are-ih-staff-who-work-together-patient-comfort-safety


IH offers a range of services to help those who may have mental health, substance use or housing needs.
/stories/sharing-warmth-and-hope-ih-health-services-help-communities


Jayme helps ensure lived experiences are not just welcomed but embedded across Mental Health and Substance Use services at IH.
/stories/we-are-ih-coordinator-centres-peer-voices-care


As temperatures drop, it’s important to be aware of the health risks of cold. Here's what you can do to ensure you remain safe and healthy.
/stories/how-protect-yourself-and-others-when-temperature-drops
STAY CONNECTED
Receive news, alerts, public service announcements and articles right to your inbox.

