Breadcrumb
Explore Stories
Health & Wellness
Guest post by Zoe Maika, a UBC Dietetics student
As dietitians, we encourage everyone to eat vegetables and fruit year-round. Fresh fruit and vegetables have long been many consumers’ first choice. But with the price of fresh vegetables up 15.9 per cent since December 2021, you may want to head to the frozen food aisle more often.
If you’re craving a crunchy apple or some fresh veggies with dip, fresh produce is the way to go. But if you want to make a nutritious meal and don’t feel like splurging in the produce section or spending time chopping, a trip to the frozen aisle is in order.
Here’s why:
Community & Culture
Name: Joanne Standish (she/her/hers)
Job Title: Occupational health nurse and safety advisor
Years of Service: 5.5
Worksite: Commerce Court / IH-wide service area
Community: Penticton
Ancestral Territory: Syilx Okanagan
Favourite Quote / Advice to live by: "Our goals can only be reached through the vehicle of a plan. There is no other route to success" - Pablo Picasso
Joanne Standish grew up in the small town of Burstall in southwestern Saskatchewan, with a “single gas plant on the prairie” as her source of livelihood in an otherwise rural farming community. After spending a year in chemical engineering Joanne realized she wanted to help others more tangibly, and shifted to a career as a registered nurse (RN). Joanne’s interest in industry continued and while working as a nurse in acute care she also began a career in occupational health and safety (OHS) in the local oil and gas industry. “I am fascinated by learning the processes of work – in any industry – and how they potentially impact the worker and their health, safety and well-being. Once that is understood, then supporting the worker and the organization so workers don’t get hurt or sick from work becomes clearer.”
With her Occupational Health Nursing Certificate, during her 35-year career Joanne has enjoyed many opportunities to learn and apply OHS principles across multiple industries. “Because my family life required frequent transfers throughout Alberta, I was able to work to full scope in meatpacking, gas processing, bitumen refining (Alberta oil sands), power generation and now health care.”
In 2017, Joanne finally made her dream move to Penticton with her sons to take full advantage of the Okanagan lifestyle, while continuing her career at Interior Health as an occupational health nurse and safety advisor.
Health & Wellness
It has been two years since Interior Health registered nurses (RNs) and registered psychiatric nurses (RPNs) began prescribing opioid agonist therapy (OAT).
In September 2020, a public health order (PHO) was issued by Dr. Bonnie Henry to enable nurse prescribing with the goal of increasing access to medication-assisted treatment and safer alternatives to the toxic illicit drug supply.
This PHO paved the way for the BC College of Nurses and Midwives and the BC Centre on Substance Use to work with the Ministry of Mental Health and Addictions and health authorities to develop the nurse prescriber scope in 2021.
Community & Culture
Diane Jules joined the Interior Health Board of Directors in January 2015. Over four terms and eight years, she has brought her insight, experience and leadership to the decisions facing Interior Health. Diane is a member of the Secwépemc Nation, Adams Lake Band and has served her Nation and community throughout the years in a number of roles.
While on Band Council, Diane oversaw the health portfolio for two years which gave her insight into health-care administration and the issues First Nations people were having within the health system. When she was approached to join the IH Board, Diane was happy to serve. “It’s been an exciting time to be involved in health,” she says. “One of my mottos in life is to take advantage of every opportunity that comes along.”
Community & Culture
The toxic drug crisis disproportionately affects Aboriginal Peoples. But accessing much needed health care continues to pose challenges for Aboriginal Peoples due to systemic racism and the lack of culturally safe care.
Ensuring health-care services are safe and free from discrimination is an ongoing journey at Interior Health. Building relationships, working to decolonize health care and health-care settings, and providing education opportunities for staff offer pathways to understanding and reconciliation.
In Creston, the Yaqan Nuʔkiy (Lower Kootenay) Band and IH staff have formed the Ki?su?k Awumu (Good Medicine) Working Group to address the needs of Aboriginal Peoples. The group came together to initiate collaborative discussions between the Band and IH staff, and now meets regularly to provide focus and direction around increasing understanding, educating staff, strengthening relationships, healing, and implementing effective ways to serve Aboriginal clients.
Creston community members join the canoe walk on Nov. 23, 2022 in support of those struggling with or affected by substance use
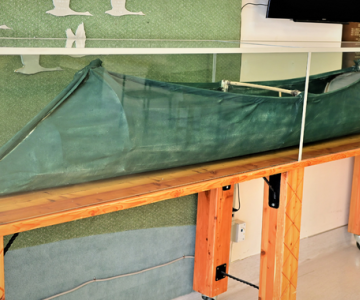
During discussions, one of the topics the group focused on was a sturgeon-nosed canoe located on the main floor of the Creston Valley Hospital. This canoe was constructed by four Ktunaxa Nation youth 10 years earlier, and was presented as a gift to the hospital during National Addictions Awareness Week on November 23, 2012. Members of the Yaqan Nuʔkiy Band carried this canoe through harsh weather along a 6 km route to the hospital to present it as part of a commitment to a healthy and healing partnership. The sturgeon-nosed canoe is “representative of life” and unique to the Yaqan Nuʔkiy Band.
Regretfully, this symbol of healing between the Band and the hospital became forgotten in an almost out of sight area of the hospital.
As clinical operations director for Creston Valley Hospital Walter Felitsyn shares, “We asked ourselves, how can we refresh and honour the significance of this gift? In consultation with an Aboriginal Patient Navigator, IH staff rediscovered how to relate our commitment to reconciliation, and honour the gift of the canoe appropriately as part of the path to healing and relationship building.”
In September 2022, Walter offered on behalf of Interior Health a gift of tobacco to Yaqan Nuʔkiy Band Nasuʔkin Jason Louie to signify the promise of renewed respect and commitment to honour this very important gift.
IH clinical operations staff, L to R: Kendra Kruger, Walter Felitsyn and Jason Schinbein.
Today, the canoe is in its rightful – and respectful – place: displayed as a central piece in the hospital lobby under museum-quality glass. Its new location has revived interest in and curiosity about the canoe from both staff and visitors. Work is underway in collaboration with Yaqan Nuʔkiy Band to establish a video display above the canoe to share its history and significance, and the Ktunaxa Nation’s culture.
Community & Culture
Name: Fiona Bradford (she/her/hers)
Job Title: Social work professional practice leader
Years of Service: 6
Worksite: East Kootenay Regional Hospital
Community: East Kootenay region – between Invermere, Kimberley, and Cranbrook
Ancestral Territory: I live and work between the Ktunaxa and Secwepemc territories
Favourite Quote / Advice to live by: We generally regret the things we didn’t take a chance on in life, rather than the things we did.
As a forester turned social worker, ultra-marathoner and team leader, Fiona Bradford brings her full focus and passion into everything she does in life.
For Fiona, social work was an intentional career choice. She originally completed a forestry degree and worked in the B.C. forest industry. Says Fiona, “I was a forester before GPS was invented, and I admit that my directional skills were not very good. I spent a lot of time looking at upside-down maps and wondering where my truck was parked!” After eight years in that profession, she realized that her heart was more suited to a people-focused career, and returned to university to pursue a bachelor and then master degree in social work.
When she and her husband decided to raise their three kids in Invermere, Fiona started a private practice, which she ran as a sole practitioner for 10 years. She then realized she wanted to work toward systemic change within a team of social workers, which led her to Interior Health. At IH, Fiona has had several different roles: she’s worked in mental health counselling; renal social work; on the regional mental health and substance use team; and now works as a professional practice leader out of the East Kootenay Regional Hospital.
Community & Culture
We know that representation matters in health care. Women play an integral role in teams within Interior Health sites, departments, projects, and education. At every level, there are contributions made by women to improve the health and well-being of our communities.
Women hold a number of key leadership roles at Interior Health including president & CEO, as members of the board of directors, and medical chiefs of staff. More than 1,000 of the physicians working at health-care facilities in our region are women.
“Within Interior Health, I think we have done quite well in this space. We have female leaders at all levels and we have wage parity,” says Susan Brown, president & CEO of Interior Health. “However, there is always room for improvement by making it easy for those who want to advance by, for example, making childcare more accessible. What is really important is that we are using our employee feedback to advance in this area."
This year the Government of Canada's theme for International Women's Day is Every Woman Counts.
“For me, it’s that not everything women do will be visible to others, or even readily acknowledged. There are a lot of working women out there who juggle full plates every day, at work and at home! It’s not always easy, but the work women do is meaningful and makes a difference to individuals and communities,” says Susan.
In honour of International Women's Day on March 8, 2023, we're profiling four of the amazing women at Interior Health.
Community & Culture
Four teens have won Interior Health’s Take a Breath: Teen Voices on Tobacco and Vaping poster contest. Each winner will receive a $150 gift card of their choice. The winning posters are being professionally printed, displayed in hospitals and health centres, and shared with schools throughout the region.
“We want to thank everyone who took the time to submit an entry for this poster contest to help raise awareness and help people make informed decisions on this important health topic,” says Interior Health medical health officer Dr. Fatemeh Sabet.
“Smoking tobacco and vaping have significant, proven negative impacts on our health. These posters by youth for youth provide important information about the health risks, and differences between commercial and traditional tobacco use.”
Community & Culture
Name: Kevin Miskosky (he/him/his)
Job Title: Maintenance Worker
Years of Service: 32
Worksite: Gateby Care Facility
Community: Vernon
Ancestral Territory: Syilx Nation
Favourite Quote / Advice to live by: “Do it once, do it right.” - Anonymous
Kevin Miskosky, maintenance worker at Interior Health, has been in B.C. health care for an impressive 32 years. Kevin started at Surrey Memorial Hospital, then moved to Vernon Jubilee Hospital in 1997, and finally to Gateby Care Facility in Vernon in 2009.
A jack-of-all-trades, when asked what keeps him motivated in his job, Kevin responds: “All my moms and dads at Gateby.” The residents are what is most important to Kevin, day in and day out.
-
Load More
Showing 414 of 675
Sign up for email updates
Receive news, alerts, public service announcements and articles right to your inbox.