Breadcrumb
- Home
- media
Explore Media
Public Service Announcement
Ashcroft and area residents are advised of temporary changes to hours at the Ashcroft Urgent and Primary Care Centre (UPCC) due to limited nursing availability.
On Sunday, Dec. 18, services will be unavailable and patients can access care at Royal Inland Hospital at 311 Columbia Street in Kamloops.
Anyone can call HealthLink BC at 8-1-1, or visit www.HealthLinkBC.ca for non-emergency health information from nurses, dietitians and pharmacists 24 hours a day, seven days per week.
The Ashcroft UPCC is normally open 8 a.m. – 8 p.m. seven days a week.
Public Service Announcement
New Denver and area residents are advised of temporary changes to emergency department hours at Slocan Community Health Centre due to limited physician availability.
Starting 8 a.m. Saturday, Dec. 17 to 8 p.m. Sunday, Dec. 18, emergency services will be unavailable, and patients can access care at the Arrow Lakes Hospital at 97 1st Ave. NE, Nakusp.
People in the community who need care due to life-threatening emergency (i.e., chest pains, difficulty breathing, severe bleeding) should always call 911 for transport to the nearest available and appropriate facility.
Anyone unsure whether an emergency room visit is warranted can call HealthLink BC at 8-1-1, or visit www.HealthLinkBC.ca for non-emergency health information from nurses, dietitians and pharmacists 24 hours a day, seven days per week.
The emergency department in New Denver is normally open 8 a.m. to 8 p.m. seven days a week.
Public Service Announcement
The best way to protect children and families from influenza is to get the influenza vaccine.
In B.C., everyone six months and older is recommended to get an annual influenza vaccine. Getting vaccinated is especially important for those at greatest risk from infection including children under five years of age, adults 65 years and older, people who are pregnant and people with chronic illnesses.
There is still time to get your infants and children vaccinated to prevent serious illness. Interior Health immunization clinics offer a choice of nasal spray influenza vaccine or the influenza shot for children.
Families with children can now drop-in at all Interior Health immunization clinics for influenza immunization and COVID-19 boosters, making it quick and easy to get immunized.
To find a clinic near you, visit the Immunization Clinics page.
As we anticipate an increase in demand, we ask that people visiting the immunization clinics be patient.
Appointments are still recommended for adults and teens. To book an appointment, visit Get Vaccinated BC.
As a reminder, children under nine years of age receiving their first-ever influenza vaccine dose will need a second dose of the influenza vaccine after four weeks. Those who have been vaccinated for influenza in previous years only require a single dose.
News Release
Interior Health and RCMP are enhancing the successful partnership programs in Kelowna and Kamloops by hiring additional staff in each community and expanding operating hours to provide this specialized crisis response service 12 hours per day, seven days per week.
“When people are in crisis because of mental illness or addictions challenges, we want them to be met with care,” said Sheila Malcolmson, Minister of Mental Health and Addictions. “Expanding the successful Integrated Crisis Response Teams in Kamloops and Kelowna will support more people in distress and connect them to help and healthcare.”
The programs in Kamloops and Kelowna, respectively known as Car 40 and the Police And Crisis Team (PACT), have a new name: the Integrated Crisis Response Teams. The programs will benefit from increased consistency in training, roles, reporting, and evaluation.
“Working together, RCMP and Interior Health are committed to addressing the needs of vulnerable people in our region. We recognize that cooperation and collaboration are critical to ensure quality care for people experiencing mental health and substance use related crises,” says Interior Health President and CEO Susan Brown. “This is a first step as we work together to enhance crisis response across the region.”
The additional staffing and expansion of hours is based on an analysis of call data. Community need will continue to be monitored to ensure objectives are being met.
“I want to commend the ongoing work of the committee, especially co-chairs Mr. Jason Giesbrecht from Interior Health, and Supt. Shawna Baher from the RCMP. Interior Health and the RCMP are committed to working together in finding solutions that support ‘persons in crisis’. Standardizing and expanding the existing Integrated Crisis Response Teams in Kamloops and Kelowna is the first step towards my vision of a model that has health clinicians available to support a police officer at every ‘person(s) in crisis’ call,” says RCMP Chief Superintendent Brad Haugli. “The RCMP want to ensure ‘person(s) in crisis’ get the help they desperately need.”
The Interior Health/RCMP Joint Committee continues to meet and work together looking at crisis response services across the region, including those in smaller jurisdictions, to identify additional opportunities for crisis response enhancement.
The Integrated Crisis Response Teams are one option within overarching crisis response services. These teams provide a specialized response to individuals experiencing a mental health or substance use crisis, when intervention by a mental health clinician is needed and there is no risk of violence. Together a specially trained officer and clinician provide short term crisis management with assessment and intervention, help with admission to hospital, connection to other medical and social services, and other supports.
“I know residents of Kamloops will be happy to hear about the expansion of this crisis response service as we continue to see many people struggling with mental health and substance use issues on our streets. This is a great step forward,” says City of Kamloops Mayor Reid Hamer-Jackson.
Kelowna Mayor Tom Dyas says today’s announcement is good news and complements other work underway in the city.
“We know that RCMP continue to face mounting mental health-related calls. Having professionals with the necessary training to deal with mental illness will help people in our community who are experiencing a mental health crisis,” he says.
Interior Health also provides Crisis Response Teams who receive phone calls from community members and existing clients who are experiencing a crisis. These teams are the main contact for RCMP for requests to provide mental health assessments, including suicide risk assessments; substance withdrawal assessments; links to Opioid Agonist Treatment if required; and referrals to community services.
Interior Health has several outreach teams who liaise with police partners on an as-needed basis. These outreach teams include Access, Treatment Support and Recovery (TSR), Assertive Community Treatment (ACT), and Substance Use Outreach.
For more information about mental health and substance use services in Interior Health visit interiorhealth.ca.
For information about the RCMP Southeast District visit the Royal Canadian Mounted Police webpage.
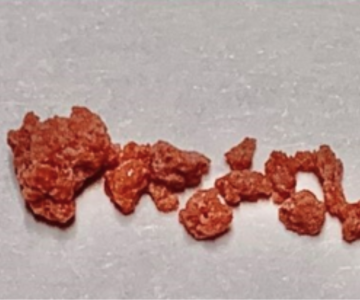
Toxic Drug Alert
Please see the attached document to learn more about the look, contamination, and risk associated with the current drug alert.
View more toxic drug, environmental, and COVID-19 alerts
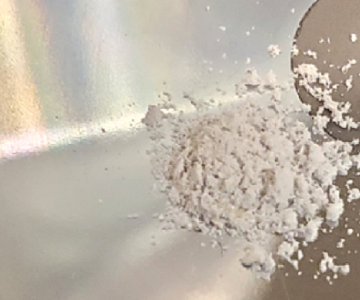
Toxic Drug Alert
Please see the attached document to learn more about the look, contamination, and risk associated with the current drug alert.
View more toxic drug, environmental, and COVID-19 alerts
Information Bulletin
Exposure to radon gas is a preventable health risk. The only way to know the level of radon gas in your indoor environment is to test for it. We encourage residents living, working and playing in the B.C. Interior region to test for radon in your homes, places of work and indoor leisure environments.
What is radon?
Radon is a naturally occurring radioactive gas without colour or odour. It comes from the ground, and it often enters and stays in buildings with low ventilation. Radon exposure is the second leading cause of lung cancer after smoking.
The BC Centre for Disease Control estimates higher radon levels in parts of the Interior region. This could potentially mean higher indoor concentrations and increased health risks. This is concerning because of the large amount of time Canadians spend indoors. Buildings generally have higher concentrations of radon gas in their lower levels (basements, ground-level main floors).
Smoking and inhaling tobacco smoke increases the cancer-causing risk of radon gas exposure. According to Health Canada, those exposed to tobacco smoke and high concentrations of radon are eight times more likely to develop lung cancer than non-smokers.
What you can do
The good news is that exposure to radon gas can be mitigated. Testing is easy and there are ways to greatly reduce radon levels if they are found to be high. Radon mitigation systems can be installed in any building. Certified radon professionals can reduce levels by over 90 per cent; a certified professional or skillful handy person following Health Canada guidance can generally complete the work within a day.
Lowering the concentration of radon in buildings and decreasing exposure over your lifetime will decrease the harmful effects linked with this gas.
Regardless of ownership of the building, anyone can test their indoor air. If high concentrations of radon are found after testing, carrying out long-term radon mitigation strategies is something generally done by the building owner.
Learn more
Find out more information about radon and your health at www.interiorhealth.ca/radon, learn more at HealthLinkBC, and visit the BC Lung Foundation to order your three-month test kit during the cold season.
Municipalities can also support radon reduction efforts by developing policies and plans around radon testing and reduction.
News Release
Supports to add more frontline Grand Forks health-care workers are now available through the Ministry of Health and Interior Health (IH) to address ongoing critical staffing challenges.
“Grand Forks faces unique challenges to staffing which require community-based solutions and thinking outside the box,” said Adrian Dix, Minister of Health. “These incentives are an important step towards bringing best practices from around the province to Grand Forks and stabilizing local health services people in the area expect and deserve.”
The incentives and resources are available to eligible frontline Interior Health Grand Forks staff who work at Boundary District Hospital, Hardy View Lodge long-term care home and in community settings such as home support and mental health substance use services.
“I know that I – and our whole community – are enormously grateful for the dedication of our nurses, doctors and other health-care professionals in delivering such high-quality care in our rural communities. These incentives recognize the increased risk patients and families face given the distances they have to travel to access other hospitals and services,” said Roly Russell, MLA for Boundary-Similkameen. “These immediate steps, coupled with the 70 actions in the health human resources strategy, will help support and stabilize health-care services in the Boundary.”
New incentives include:
Up to $2,000 in a quarterly retention bonus for eligible existing staff depending on how much they work (maximum amount for full-time). This is an expansion of the existing Provincial Rural Retention Incentive (PRRI) program currently being prototyped by communities in Northern Health.
1.5 times normal wage for staff who travel more than 40 kilometres from other IH worksites to support services in Grand Forks.
Up to a $1,500 bonus for Interior Health staff referring other health-care workers to Grand Forks who sign on to eligible positions.
Extension of Northern Health’s Travel Resource Program (TRP) to include Grand Forks which will provide access to a pool of nurses to support the community. TRP nurses can begin to request and schedule shifts in Grand Forks beginning December 1.
Limited staffing resulted in the temporary closure of inpatient beds at Boundary Hospital in March. To date, emergency department services have gone above and beyond to avoid more significant closures, but additional staff are also required to stabilize emergency services and reduce the risk of any interruptions.
“These incentives are part of our commitment to local patients and to our current staff and physicians who remained steadfast in their dedication to Grand Forks and Boundary communities during these challenging times,” said Dr. Shallen Letwin, vice president of clinical operations, IH South.
Incentives are currently available for the following positions:
Registered Nurse
Registered Psychiatric Nurse
Licensed Practical Nurse
Health Care Assistant
Community Health Worker
Medical Laboratory Technologist
Medical Laboratory Assistant
Radiology Technologist
Social Worker
Occupational Therapist
Physiotherapist
Sonographer
Dietician
Frontline Clinical Managers (Referral Bonus and PRRI only)
Incentives will come into effect immediately and Interior Health will be sharing additional details with staff and unions to ensure eligible individuals are aware and can access them appropriately.
News Release
As the toxic drug crisis continues, Interior Health in collaboration with local prescribers has implemented a new model to help connect people in the East Kootenay region who have opioid use disorder with opioid agonist treatments (OAT), such as methadone and Suboxone.
“When people bravely reach out for help, we want supports to meet them,” said Sheila Malcolmson, Minister of Mental Health and Addictions. “This innovative approach will help more people in the East Kootenays access life-saving treatment, as government continues to build a system of mental health and addictions care across the province.”
A new centralized East Kootenay-wide OAT clinic has been launched in order to maximize OAT prescribing resources in the region. The clinic provides clients with access to an OAT prescriber on any weekday at their local Mental Health and Substance Use (MHSU) centre, using an innovative blend of in-person and virtual appointments.
The service is available in five East Kootenay communities: Cranbrook; Creston; Invermere; Golden; and Sparwood.
The clinic is comprised of physicians, nurse prescribers and a centralized medical office assistant.
“The provision of OAT medication, and with substance use treatment generally, has unique challenges. By leveraging technology and through working together we continue to remove barriers to treatment. I’d like to thank the prescribers who have stepped up to participate in this program, while encouraging others to do so as well,” said Interior Health president and CEO Susan Brown.
This new model is a unique approach to address several challenges presented by the geography of the region. It also provides more options for clients whose prescriptions run out, who may otherwise rely on illicit opioids.
Call the new OAT intake office at 250-420-2210.
Earlier this year, Interior Health announced a project to connect people with opioid use disorder with Suboxone in hospital emergency departments.
To learn more about OAT medications in the treatment of opioid use disorder visit our OAT page.
Quotes
David
“Personally it has given me my life back. It was taken away when I had my accident, and again when I became addicted to the pain meds I needed. OAT therapy has taken away the cravings and desire for any other meds because I am now on the right med at the right dose. I am not stigmatized by the physician and we have built a good relationship. Virtual visits have been helpful. I am able to have a physician who does not live in my own community and get the care I need.”
Lisa
“I would like to share what the OAT program has done for me. For many years under a doctor’s care I was on Oxycodone and needed to come off. I was in the hospital for three weeks and it was the worst thing I ever went through. The Nurse Prescribers at the OAT program were vital in my recovery as I have stayed clean for a year now and don’t know what I would have done without them. They are so caring and invested in my recovery that I feel I can share anything with them and they have done everything in their power to suggest support, listen and encourage. I know they are probably overworked, but they never turn their backs. They are wonderful at what they do, and without them, I may have given up and relapsed. Instead, I am very proud to say I have a year in recovery. I could never repay what they have done for me, and in today’s world someone who sincerely cares is rare. I would recommend this program to anyone and feel blessed to have this resource.”
Jaime
“I’ve been coming to the OAT clinic almost a year now and it has helped me change my life. The Nurse Prescribers there are easy to talk to, understanding and non-judgemental. With their help and knowledge of what medications would help my withdrawals, they helped find the right program. I am on the Sublocade (buprenorphine) program, and with it I was able to get my life back to normal rather than depending on something everyday just to get me through. I’m able to spend time with my kids and not have to worry about appointments every day. I definitely would not have been able to beat my drug habit if there was no clinic like this to go to. Thank you sooo much.”
-
Load More
Showing 621 of 1113