Breadcrumb
Explore Stories
Health & Wellness
A person can bleed to death from an injury in as little as five minutes. That means every second counts when it comes to stopping uncontrolled bleeding, and anyone – a friend, family member or even a bystander – can help save someone’s life.
Think of it as you would with basic first aid, CPR or the Heimlich Manoeuvre – knowing the steps to getting bleeding under control fast can significantly increase a person’s odds of survival.
Traumatic accidents can happen anywhere – in the kitchen or garage, in a motor vehicle, or during outdoor recreational activities such as cycling or hiking. No matter how safe you are trying to be, everyone is at risk of potential injury, which can result in bleeding from extremities such as the neck, groin, armpits, chest and abdomen.
That’s where an initiative such as Stop The Bleed comes in.
In a nutshell, Stop the Bleed trains people how to stop a person from bleeding to death. It was initiated by the American College of Surgeons in 2015 after the active shooter event at Sandy Hook Elementary School in Newtown, CT. Stop the Bleed has been adopted by Trauma Services BC to help teach basic life-saving skills to health-care professionals and members of the public.
“Bystanders or loved ones are often in the best position to provide early assistance to an injured person who is bleeding. Having the skills, confidence and basic equipment to stop someone’s bleeding early can mean the difference between life and death,” says Kyla Gowenlock, Interior Health’s network director for Trauma Services. “I encourage everyone to take the Stop The Bleed course and stock their car or backpack with the basic equipment. Anyone can be trained to save a life.”
Community & Culture
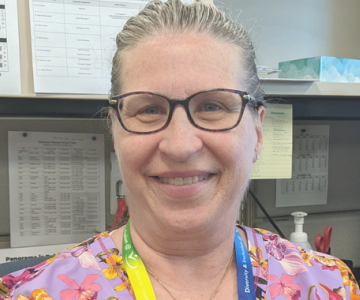
Name: Tanya Chmilar (she/her/hers)Job Title: Registered Nurse/Registered Psychiatric NurseYears of Service: 25Worksite: Community Health Services CentreCommunity: KelownaAncestral Territory: Syilx OkanaganAdvice to live by: Have fun and do your best. Maintain a work-life balance.
Tanya Chmilar lives her motto every day — both at work and in her personal life: Have fun and do your best. After earning her Psychiatric Nursing Diploma in 1985, and her General Nursing Diploma in 1988, Tanya worked in Vernon, Kelowna and Cranbrook psychiatric inpatient units. She moved to Vancouver to complete her BScN from the University of British Columbia (UBC), then worked in emergency and short stay psychiatry at St. Paul’s Hospital and UBC.
Community & Culture
Name: Jana Schulz (she/her/hers)Job Title: Regional Dementia Education Coordinator, East KootenayYears of Service: 7 monthsWorksite: Rocky Mountain LodgeCommunity: CranbrookAncestral Territory: Ktunaxa Nation
Jana Schulz was born and raised in Cranbrook, B.C. In less than a year at Interior Health (IH), she has made a big impression as the Regional Dementia Education Coordinator for the East Kootenay, based at Rocky Mountain Lodge in Cranbrook.
“She does a wonderful job, and is very much appreciated by her colleagues on the regional Seniors Mental Health team,” says her co-worker, Cherylynne Greenard-Smith. “Her courage to speak up and give recommendations for fair and culturally sensitive treatment of Indigenous Peoples is incredibly helpful to the work that we do, and also admirable and inspiring.”
Research & Innovation
Navigating a conversation about an individual’s serious illness can be a difficult and uncomfortable part of the job for many health-care providers. Some may be unsure about what to ask, or how much detail to share with someone about their condition and prognosis.
Yet, having open, honest and compassionate conversations with people during their illness is essential to help individuals and families make care decisions that align with their personal goals, hopes and wishes.
Within Interior Health, providing support for staff and physicians by having Serious Illness Conversation Guide workshops has been a priority for several years. Online education tools and role play opportunities help clinicians feel more comfortable navigating these essential conversations.
“Research in cancer care is clear. Person-centred communication gives less anxiety, less depression and on average a longer lifespan. Imagine this approach applied to both preventing and living with chronic disease. No side effects. Only benefits for all involved,” says Dr. Greg Andreas. “It is time to change. Care should be first about the person, not their pathology. Planning can then evolve for their best possible days, months, decades… I have yet to have anyone talk about how they would like to spend their last 12 months of life lost in our hospital system.”
Practice lead Carla Williams agrees and says she believe when clinicians use the Serious Illness Conversation Guide and talk about a person’s wishes early on, it improves the individual’s experience of death and dying.
She recalls how the guide helped her in a conversation with a woman who was palliative in hospital.
“Staff were uncomfortable because they said she did not believe she was dying but they felt that hospice would be best for the patient,” says Carla. “I introduced myself as a social worker, (and) let her know that I was here to ask for permission to have what we call a Serious Illness Conversation to better understand her wishes relating to her health.
“I asked ‘what is your understanding of where you are today?’ She very clearly stated, ‘I am dying and have a month to live.’ We continued through the discussion asking about her goals, fears, strengths, abilities, trade-offs and family. At the end of the discussion, she was clear that she wanted to go to hospice and have her family with her. She already knew she was dying and knew where she wanted to palliate and felt comfortable knowing she would not undergo more testing and have a lengthy hospital admission.”
Carla says the Serious Illness Conversation Guide is especially helpful because the language is so clear.
“In my experience with using the guide, I have never had a patient not understand the questions as they are written. There has never been a time when a patient expressed confusion over the question when using the guide as it recommends. I believe that the patient-tested language is powerful and that the questions truly illicit the true feelings and desires of the patient as they move through their own mortality,” says Carla.
In Interior Health, the work to build capacity for Serious Illness Conversations and develop a community of practice has been led by clinical nurse specialists Vicki Kennedy and Shannon Paul-Jost. Vicki’s work is in palliative and end-of-life care, while Shannon’s focus is gerontology. They were early adopters, having participated in a BC Centre for Palliative Care’s Serious Illness Conversation Guide Train the Trainer workshop in 2018.
Two pilot Serious Illness Conversation Guide workshops were conducted across the Interior Health region, and an evaluation showed positive results that clearly demonstrated the value of the guide. This led to the development of a knowledge translation strategy, and to the building of relationships with post-secondary institutions across the region. Today, faculty from UBC Okanagan, Thompson Rivers University, Selkirk College and College of the Rockies have all expressed interest in workshops for third- and fourth-year nursing students.
Since July 2018, there have been 43 Serious Illness Conversation Guide workshops in Interior Health, with 891 individuals trained to have Serious Illness Conversations.
Learn more:
Visit our Advance Care Planning page
Visit our Palliative and End of Life Care Overview page
Community & Culture
Shawna Biron, far right, with colleagues (L-R) Debbie Whitehead, Shannon Statham and Terri Domin at a recent Ktunaxa Nation Letter of Understanding meeting.
Community & Culture
Sewing the symbolic ribbon skirts for Indigenous volunteers at this year's International Overdose Awareness Day events in Kelowna
Kori Smith is the mother of two young children, and expecting her third. Born in Portage la Prairie, Man., treaty to Long Plain First Nation, she is of Ojibwe and Cree ancestry. She now lives in Kelowna.
As a member of KANDU (Knowledging All Nations and Developing Unity) and a peer advisor for Interior Health’s mental health and substance use network, Kori understands the importance of International Overdose Awareness Day.
“August 31 is an important day for me because I have family who have overdosed in the past. One who has since passed away and the other who is still addicted to drugs,” says Kori. “It is a great way to spread awareness and be there for the ones we care about and love and to remind them that they are not forgotten.”
With support from the mental health and substance use network, Kori and her sister have sewn 10 purple ribbon skirts for Indigenous peer volunteers to wear for the Kelowna International Overdose Awareness Day events.
“I recently started ribbon skirt making by learning from my koko (grandma) Lorraine Daniels. She is a residential school survivor and is also the executive director of the National Residential School of Canada in Portage la Prairie, Man.,” explains Kori.
Community & Culture
Dr. Anders Ganstal enjoying his favourite winter activity - skiing
Name: Dr. Anders Ganstal (he/him/his)Job Title: Emergency Physician, Clinical Assistant Professor for UBC Department of Emergency Medicine, Regional Medical Director for the British Columbia Emergency Health Services (BCEHS) InteriorYears of Service: 17Worksite: Royal Inland HospitalCommunity: KamloopsAncestral Territory: Tk'emlúps te SecwépemcFavourite Quote/Advice to live by: Live for today, plan for tomorrow
With the ultimate goal of improving patient care, Dr. Anders Ganstal leverages his local and regional leadership roles to advance large-scale health-care initiatives. Referencing one of his favourite sports, Anders shares, “Quality improvement is similar to mountain biking. When you look up to the top from the bottom, it’s quite overwhelming. It’s one step at a time; that’s how you get to the top of the mountain.”
For this physician leader, it’s the contribution of every single person and each incremental step in the right direction that help push a change initiative forward.
Community & Culture
Senior woodworking students at Clearwater secondary participated in a project to build keepsakes for parents who lose babies at birth
A short lifetime of memories are attached to a project undertaken by Clearwater woodwork students last spring for grieving parents at Royal Inland Hospital.
For the students who carefully handcrafted the beautiful memory boxes, it taught knowledge and skills and also compassion in the face of deep sorrow.
For parents leaving the hospital with only memories of a baby, it provides a beautiful, engraved keepsake – a place to store tangible remembrances like photographs, clothing or tiny hand and foot prints.
Clearwater secondary school teacher Dayton Fraser was first approached about the woodworking project by a colleague whose daughter, Keira Geiger, was a nurse working on a preceptorship (practical experience and training) in the obstetrical unit (OB) at Royal Inland Hospital (RIH).
The idea was to build memory boxes and donate them to the hospital where they could be given to parents going home with only a broken heart.
Dayton, who is always on the lookout for projects that will engage students and teach them their craft, eagerly embraced the concept.
“It was a great project for our senior woodworking students. It got them on every machine from table saws to lasers for engraving and it gave them insight into life circumstances,” he said.
“It’s such a tragedy to lose a child and these students were really motivated to build a beautiful keepsake that these parents would be able to cherish forever.”
Fifteen students participated in the project and they did an “awesome job.” Each one is engraved with a butterfly and some other design, such as a baby toy or teddy bear.
Dayton said it took longer than anticipated and not every student completed their box, but those boxes will go into the inventory for next semester.
As the project progressed, Keira completed her preceptorship and Dayton remained in contact with the OB clinical practice lead, Val Kloska. In July, she was excited to get a call from him, saying he was ready to drop off the first instalment of the memory boxes.
When he arrived at the new labour and delivery unit in the Phil & Jennie Gaglardi Tower, he was met enthusiastically by Val and the labour and delivery team who understand just how much the boxes will mean to devastated parents.
“It was such an amazing project for both the school and the obstetrical unit,” said Teressa Allwood, clinical operations manager, maternal and child services. “These memory boxes will support our families during the hardest times of their lives.”
The project will continue during the next school year and be more streamlined.
“I’ve been able to fine-tune the process for next year. The first time I do a project, I’m learning the whole time,” said Dayton.
The project also epitomizes community, which is important for Dayton as a teacher.
The wood came from the property of a retired doctor, known in Clearwater as “Dr. Bob” (MacKenzie).
During COVID when students were not in school – with Dr. Bob’s consent – social studies teacher Sylvain Menard and Dayton took down the trees, which was on the path of the Trans Mountain pipeline. Dayton, metalwork and automotive teacher Bryn Leary, and retired woodworking teacher Brent Buck milled it with Brent’s portable sawmill.
Dayton views the memory box concept as reflective of the philosophy he learned from his predecessor, Brent.
“We teach our kids skills and knowledge, but what is the point if we are not using those skills and knowledge to give back to our communities?”
Community & Culture
Wanda (in the blue shirt) and her family
Name: Wanda Handschuh (she/her/hers)Job Title: Health Services for Community Living (HSCL) Nursing, Clinical Educator RNYears of Service: 30Worksite: Day-Break Adult Day CentreCommunity: VernonAncestral Territory: Syilx Okanagan / Okanagan Interior SalishAdvice to live by: “If you are going through hell, just keep going,” and “Normal is only a setting on a dryer.”
Wanda Handschuh has spent her entire life in British Columbia. Born in Dawson Creek, Wanda has also lived in Hudson Hope and Mica Creek, then Kamloops to complete school, study nursing and get married. After living in Revelstoke for a year with her husband, Darren (together for 34 years now), they moved to Vernon in 1991 and have never left.
Wanda enjoys supporting people with their health. Making people comfortable and sharing a laugh is important to her in her work. Currently a Clinical Educator in Health Services for Community Living (HSCL), Wanda enjoys meeting new people, and working with clients and their caregivers.
“Nursing has been a perfect fit for my personality and my passion. I look forward to continuing to learn about myself and others on this life journey.”
-
Load More
Showing 468 of 834
Sign up for email updates
Receive news, alerts, public service announcements and articles right to your inbox.